What is Medi-Cal Out-of-Pocket Expense Reimbursement (Conlan)?
https://www.dhcs.ca.gov/conlan
California has a program (stemming from the Conlan v. Shewry litigation) that allows Medi-Cal beneficiaries to seek reimbursement for out-of-pocket medical or dental costs they paid, under certain conditions.
Key eligibility conditions include:
• The service must have been a Medi-Cal–covered service, on a date when the person was Medi-Cal eligible.
• You must have paid out of pocket (or someone paid on your behalf).
• The provider must have been a Medi-Cal provider on the date the service was provided.
• The claim must be submitted within certain time limits (e.g. within one year of service or 90 days after issuance of Medi-Cal card, whichever is longer) for services on or after November 16, 2006.
If all criteria are satisfied, Medi-Cal may reimburse you through one of these:
1. Voluntary Provider Reimbursement (provider refunds you)
2. Involuntary Provider Recoupment (Medi-Cal recovers the cost from the provider)
3. Medi-Cal reimbursement up to Medi-Cal rate (if provider can’t or won’t pay)
So if your child’s co-pay was for a service that would be covered by Medi-Cal, and the provider qualifies, then yes — in theory you could get reimbursed under this scheme.
How the DDS / Regional Center / DD Waiver factors in?
Because your child is a Regional Center consumer and has a DDS waiver (a DD or HCBS waiver), things get more intricate.
• Having the DD waiver means Medi-Cal can cover certain services the regional center provides (or helps coordinate) as part of the developmental disability services framework.
• But that doesn’t automatically make every private-insurance co-pay eligible for reimbursement, especially if the private plan’s co-pay was for services not strictly “Medi-Cal covered” under the rules, or by a provider not enrolled in Medi-Cal.
• Regional centers may sometimes assist with co-pay assistance (depending on your household income, the regional center policies, etc.). The Process can be found here.
• Even when regional center funding or assistance is possible, it’s often a “payer of last resort” — meaning everything else must be exhausted first (insurance, Medi-Cal reimbursement, etc.).
In short: being a consumer with a regional center + waiver helps your case in terms of access and coordination, but it doesn’t guarantee reimbursement of private co-pays.
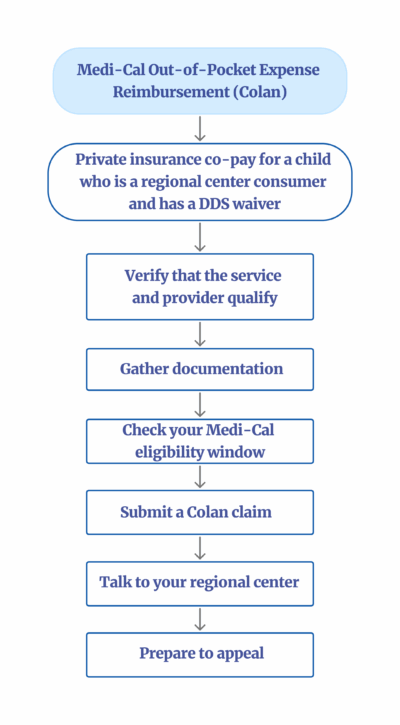
The Process
1. Verify that the service and provider qualify.
• Was the service one that should be covered by Medi-Cal?
• Was the provider a Medi-Cal–approved provider on the date of service?
• Did you or someone pay the co-pay out of pocket?
2. Gather documentation.
• Receipts, bills showing the co-pay, explanation of benefits (EOB) from private insurance, proof of Medi-Cal eligibility at that date.
• Provider statements about refusing to reimburse you for a service Medi-Cal should have covered.
3. Check your Medi-Cal eligibility window.
• The service must have been rendered during a period when you were covered by Medi-Cal (or within the retroactive eligibility window).
• If the service was before your Medi-Cal became active, see if retroactive eligibility applies (and was approved) for those dates.
4. Submit a Conlan claim.
• Fill out the Medi-Cal out-of-pocket reimbursement (Conlan) claim forms.
https://www.dhcs.ca.gov/services/medi-cal/Pages/Online-Conlan-Claim-Forms.aspx
• Submit via mail (or other method if allowed) to the DHCS Beneficiary Services Center.
Mail the completed Conlan claim packet to the Department of Health Care Services (DHCS) at:
Beneficiary Service Center
• Make sure it’s within the allowed deadline (1 year from service or within 90 days after card issuance, whichever is longer).
• If a provider refuses to reimburse, Medi-Cal can attempt recoupment from the provider.
5. Talk to your regional center.
• Ask your service coordinator whether the regional center can cover that co-pay (or a portion) in “payer of last resort” fashion.
• Ask whether your regional center’s policy allows co-pay assistance for the particular service and provider you used.
• If regional center does provide it, get the procedure and forms.
6. Prepare to appeal.
• If Medi-Cal denies your request, you have the right to request a hearing (state hearing) within 90 days of the notice. This information can be found on the back of the notice of action letter.
• Also, if the regional center denies co-pay assistance, you may need to appeal via regional center or under your Lanterman Act rights.
For children with special needs in California, Medi-Cal provides a broad set of benefits, especially if the child is also receiving services through Department of Developmental Services (DDS) and has a waiver (e.g., DD/HCBS waiver). These services go well beyond standard pediatric care. Below is a rundown of the most common Medi-Cal covered services relevant to children with developmental disabilities or complex medical needs.
Core Medical Care
• Primary Care: routine checkups, sick visits, immunizations.
• Specialist Care: pediatric neurology, genetics, developmental-behavioral pediatrics, gastroenterology, pulmonology, endocrinology, orthopedics, etc.
• Hospital Services: inpatient and outpatient care, surgeries, ER visits.
• Durable Medical Equipment (DME): wheelchairs, gait trainers, walkers, standers, communication devices, etc.
Therapies
• Speech Therapy (ST)
• Occupational Therapy (OT)
• Physical Therapy (PT)
• Feeding and swallowing therapy
• Behavioral therapies (see ABA below)
Behavioral and Mental Health
• Applied Behavior Analysis (ABA)
o For children with autism or related conditions.
o Must be medically necessary and prescribed by a physician or psychologist.
• Mental/behavioral health therapy (individual, family, group)
• Psychiatric evaluations and medication management
• Crisis stabilization and inpatient psychiatric care if required.
In-Home and Long-Term Care Supports
• In-Home Supportive Services (IHSS): personal care assistance, protective supervision, paramedical services.
• Home health nursing (e.g., LVN/RN support for medically fragile children).
• Private duty nursing when medically necessary.
Medications and Supplies
• Prescription medications (brand or generic, if medically necessary).
• Over-the-counter medications if prescribed.
• Incontinence supplies, feeding supplies, tracheostomy care, respiratory supplies, etc.
Dental and Vision Care
• Preventive and restorative dental services through Denti-Cal.
• Vision exams and glasses through the Vision Care benefit.
• Orthodontia if medically necessary (e.g., for cleft palate, craniofacial anomalies).
Transportation
• Non-emergency medical transportation (NEMT): gurney, wheelchair van, or ambulance when required for medical reasons.
• Non-medical transportation (NMT): mileage, gas, bus passes to get to appointments.
Case Management & Care Coordination
• Targeted Case Management (TCM) for medically fragile children.
• Regional Center coordination for children with DDS waiver.
• Managed Care Plan care coordinators for children with multiple needs.
Special Programs
• California Children’s Services (CCS) for children with qualifying medical conditions (e.g., cerebral palsy, congenital heart disease).
• EPSDT Supplemental Services: anything medically necessary to “correct or ameliorate” a condition, even if it’s not normally covered for adults.
• Respite services through IHSS or Regional Center (not directly Medi-Cal, but waiver-linked).
Waiver-Based Enhancements
For children on the Home and Community-Based Services Waiver for the Developmentally Disabled (DDS Waiver):
• Expanded access to Medi-Cal regardless of parental income.
• Streamlined authorization for home-based nursing and personal care.
• Supplemental habilitation or day services.
• Increased respite and transportation support